Imagine opening your lab report at 24 and seeing a number you associate with a later stage of life. An HbA1c of 6.0. No dramatic symptoms, no immediate crisis, just a quiet signal. For many young adults today, this is where the journey of insulin resistance reversal begins, long before diabetes is ever discussed.
Decades of medical research show that the process usually starts much earlier, at a cellular level. Insulin resistance is a functional metabolic state shaped by modern living, and in many cases, it is reversible.
India has long been described as the diabetes capital of the world, not as a label, but as a reflection of scale. According to the World Health Organization, an estimated 77 million Indian adults are living with type 2 diabetes. Millions are already in a prediabetic state, often without any awareness. As a result, markers of metabolic syndrome are now appearing earlier than they once did.
Over 32+ years, I have worked across healthcare communication and studied how scientific insight translates into everyday behaviour. This in-depth article is grounded in extensive clinical research and the collective work of healthcare providers globally. It takes a root-cause, lifestyle-first, science-aligned approach. We also share practical steps that help reverse it naturally.
Also Read:
- Insulin Resistance & Prediabetes: All you need to Know
- Elevating Health and Emotions: Food’s Remarkable Role in Modern Medicine
What Is Insulin Resistance — and Why It Matters Now
Insulin resistance is not permanent damage. It is a functional metabolic shift shaped by modern living. The issue is not sugar alone, but how efficiently the body responds to insulin, which explains both its silent progression and why it matters now.
What Is Insulin Resistance?
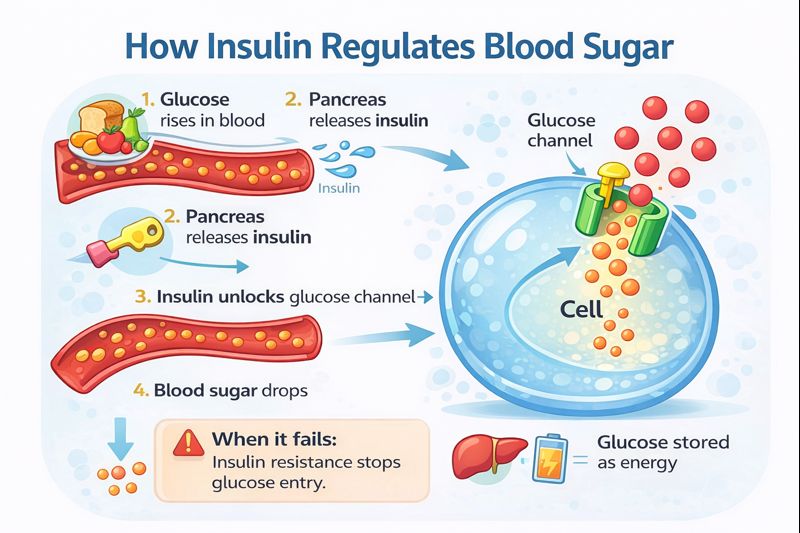
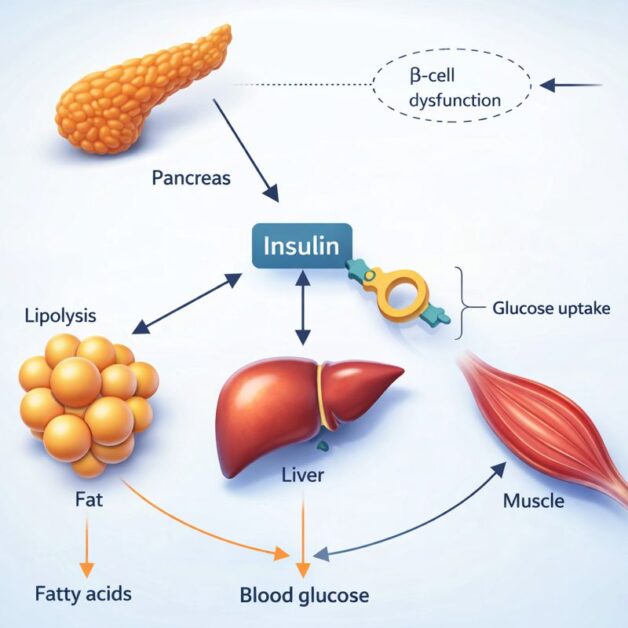
Insulin is the hormone that helps move sugar from the bloodstream into the cells, where it is used for energy. In a healthy system, this process is smooth and efficient. With insulin resistance, cells begin to respond less effectively. Sugar struggles to enter, so the body compensates by producing more insulin.
While insulin resistance is a hallmark of prediabetes and type 2 diabetes, it can also affect people living with type 1 diabetes- American Diabetes Association

As Karen Patino a metabolic educator explains, “when carbohydrates are eaten, they break down into sugar and enter the bloodstream. Insulin acts as the key that allows this sugar to enter the cell and be used for energy. With insulin resistance, that key becomes less effective, forcing the body to release more insulin to achieve the same outcome”.
“Many people are metabolically obese — they may look healthy on the outside, but internally, visceral fat and insulin resistance are driving disease long before blood sugar rises.” — Dr Robert Lustig, Pediatric Endocrinologist
This hidden fat accumulation explains why blood sugar can remain normal for years. Insulin compensates quietly, masking dysfunction. We next explore how metabolism can struggle long before standard glucose markers change.
Why Sugar Can Look “Normal” While Metabolism Struggles
In the early stages of insulin resistance, fasting glucose often remains within the normal range. This does not mean metabolism is healthy. It means insulin is compensating aggressively to keep blood sugar controlled.
As Mahima Setia, Founder Healthy Boots has highlighted through clinical interpretation, this masking effect can persist for years. During this phase, other markers often shift first. The image shows example of early insulin resistance: normal fasting glucose with elevated triglycerides and liver enzymes.
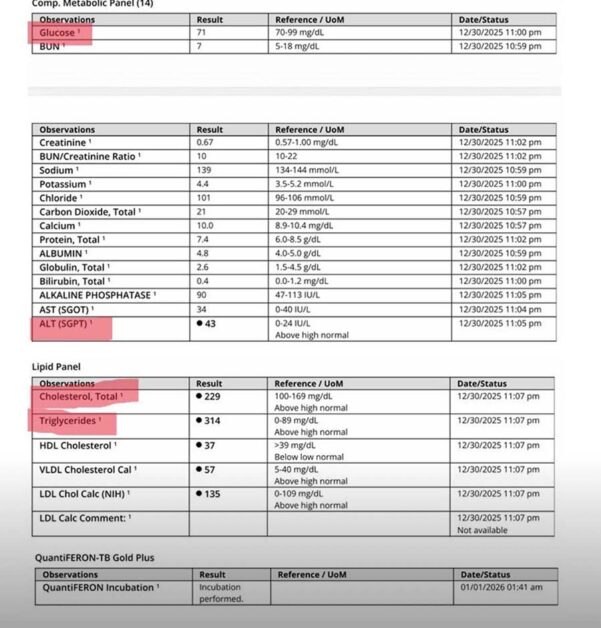
Despite normal fasting glucose, triglycerides and liver enzymes rise early, reflecting hidden metabolic stress and hepatic insulin resistance long before HbA1c or overt diabetes changes appear
Why Insulin Resistance Is Reversible
Insulin resistance is functional, not structural. Cells have not failed. They have adapted to constant insulin exposure. When insulin demand is reduced, cellular sensitivity can improve over time.
“Insulin resistance is the root cause behind diabetes and many lifestyle disorders. When you work on improving insulin sensitivity, the body begins to heal, and true reversal becomes possible.” — Dr Pramod Tripathi, Diabetologist
Early Symptoms of Insulin Resistance Most People Ignore
Insulin resistance rarely announces itself loudly. Long before blood sugar crosses diagnostic thresholds, the body sends quieter signals. Noticing these early patterns can help intervene before deeper metabolic damage sets in.
- Stubborn visceral belly fat: A firm, central weight gain that resists diet changes.
- Expanding waistline: Over 35 inches in women and 40 inches in men, even without major weight gain.
- Skin tags: Small growths around the neck, underarms, or groin.
- Darkened skin folds: Especially around the neck or elbows, known as acanthosis nigricans.
- Chronic skin issues: Acne, eczema, rosacea, or psoriasis that flare repeatedly.
- Hair thinning in women: Diffuse thinning rather than patchy loss.
- Post-meal fatigue: Feeling sleepy or drained after eating.
- Persistent cravings: Especially for refined carbohydrates.
- Difficulty fasting: Early hunger, irritability, or weakness.
- Brain fog and low endurance: Reduced focus and quicker physical fatigue.
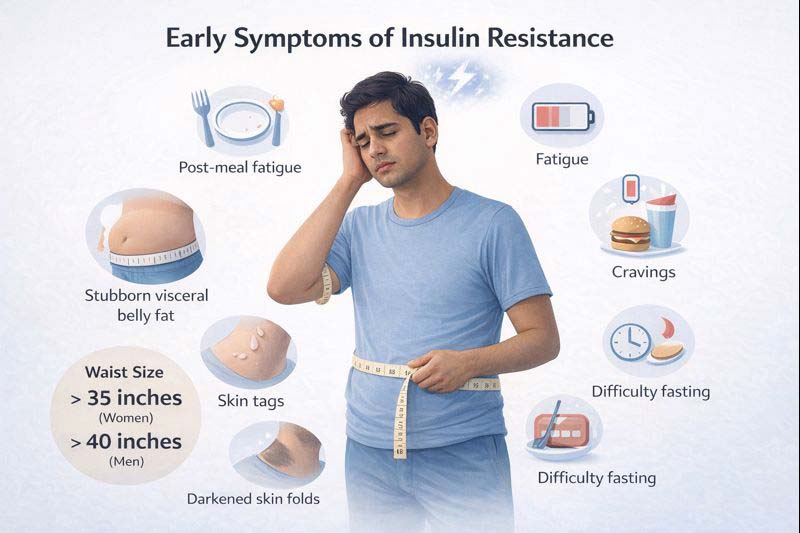
These signals are often dismissed as stress or lifestyle fatigue. In reality, they are early metabolic messages asking for attention.
Why Young Adults (around 20–25 years) Are Showing HbA1c Around 6
An HbA1c around 6.0 in the early twenties is rarely a sudden disease. It reflects early metabolic ageing, where lifestyle patterns quietly outpace the body’s ability to regulate glucose, long before symptoms feel serious.
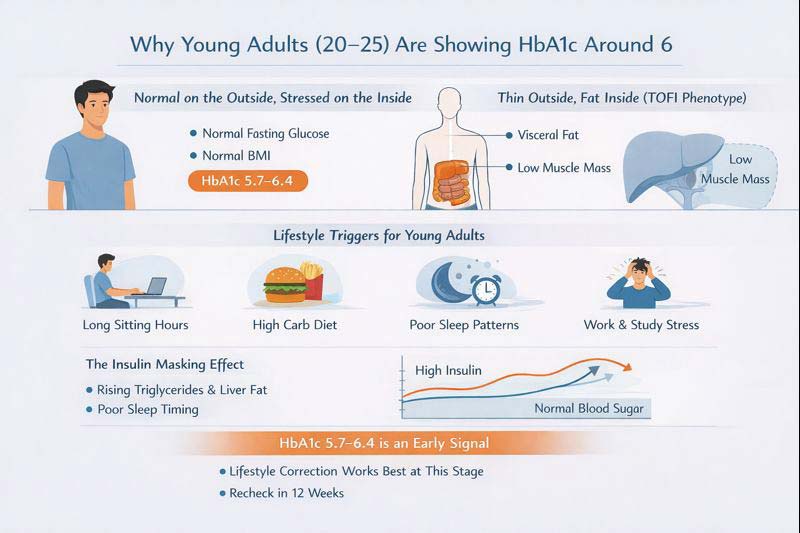
Why does HbA1c rise early even when weight looks normal?
Because weight alone does not reflect metabolic health. Many young adults follow a TOFI pattern1. Thin Outside, Fat Inside. Visceral fat accumulates around organs while overall weight stays stable. At the same time, low muscle mass reduces the body’s ability to absorb glucose efficiently.
A persistent protein gap worsens this imbalance. Muscles are not built or maintained, while refined carbohydrates remain frequent. Add long sedentary days, minimal movement between meals, and chronic sleep debt, and insulin must work harder to keep blood sugar controlled. HbA1c rises slowly, even though the mirror suggests everything is fine.
Fatty Liver Is the First Domino
The liver2 is often the first organ to struggle under excess insulin and glucose load. Fat begins to accumulate quietly, long before routine scans or symptoms raise concern. From here, insulin resistance spreads outward to muscles and fat tissue.
“Diabetes does not begin suddenly. Insulin resistance troubles the liver first, leading to fatty liver. From there, it spreads insulin resistance to the rest of the body, progressing silently from prediabetes to diabetes over years.” — Dr Brij Mohan Arora, Diabetes Specialist and Metabolic Disease expert
Prediabetes, then, is not the body screaming. It is the body whispering. An HbA1c in this range is not a verdict. It is an early conversation the body is trying to start. What follows are practical steps that translate these early signals into daily actions that lower insulin demand.
Step 1️⃣ – Movement That Lowers Insulin Demand
Modern metabolism struggles less from what we eat and more from how little we move. Long sitting hours reduce the body’s ability to handle glucose efficiently. Movement, even in simple forms, lowers the amount of insulin required to manage blood sugar.
Muscles Are the Body’s Largest Glucose Sink
3Skeletal muscle is the body’s primary site for glucose disposal. When muscles contract, they pull glucose directly from the bloodstream, often with minimal insulin involvement. This is why movement has an immediate metabolic effect and why inactivity quietly raises insulin demand.
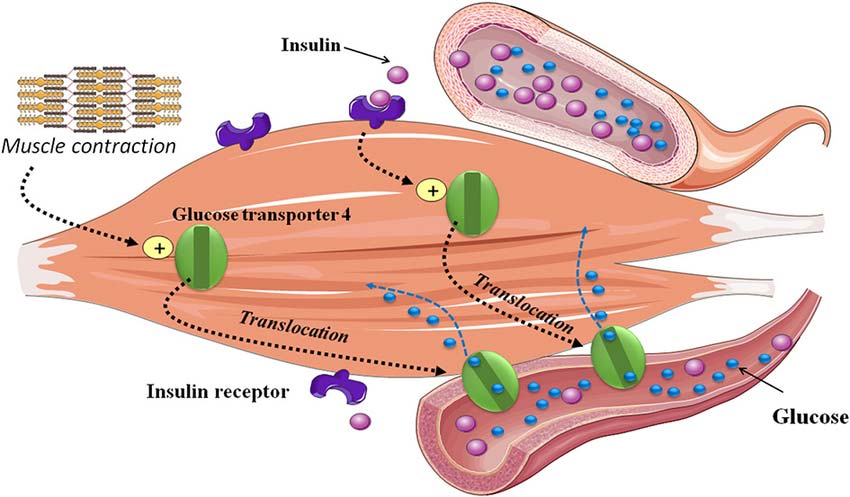
As Karan Sarin author of Sick Nation, often point out, low or underused muscle mass creates a metabolic bottleneck. Glucose has fewer places to go, so the pancreas compensates by releasing more insulin to keep blood sugar stable. Dr Sarwat Makkani, Board Certified Physician at Katy Fulshear Internal Medicine, Texas, similarly emphasises that muscle contraction itself improves glucose uptake and reduces the hormonal burden on the body.
This process has little to do with intensity or aesthetics. It is about metabolic capacity. Regular use of muscle improves insulin sensitivity at a cellular level and lowers the need for constant insulin signalling over time.
Walking After Meals (Timing > Intensity)
Movement timing matters as much as movement itself. Light activity soon after meals prevents sharp glucose spikes.
Just 2 minutes of walking after eating can help blood sugar- NIH
Research insights highlighted by Leidien Treur show that a short walk after meals can blunt post-meal glucose excursions effectively. Just 10 to 15 minutes of relaxed walking helps muscles absorb incoming glucose before it overwhelms the system. No special gear. No high intensity. Consistency matters more than pace.
Think of it as clearing traffic before congestion builds. When glucose is handled early, insulin does not need to surge later. Over time, this simple habit lowers baseline insulin demand.
Step 2️⃣ – The Insulin Resistance Diet (Without Extremes)
Diet plays a central role in insulin resistance, but not in the dramatic, all-or-nothing way it is often presented. For most people, the issue is not eating one “wrong” food. It is how often insulin is triggered and how large the spikes are.
Is cutting carbs the fastest way to reverse insulin resistance?
No. Cutting carbohydrates is not the first or most effective step for most people. What matters more initially is sequencing and balance. Pairing carbohydrates with adequate protein, fibre, and fats slows glucose absorption and reduces insulin spikes. Only when this foundation is in place does carbohydrate reduction become useful.
In healthcare communication work, I have repeatedly seen confusion arise when people remove carbohydrates aggressively without fixing meal structure.
The “Two Buttons” That Matter Most
Health experts often explains diet using a simple but effective analogy. A simple way to understand this is to focus on two levers that every meal presses, whether intentionally or not.
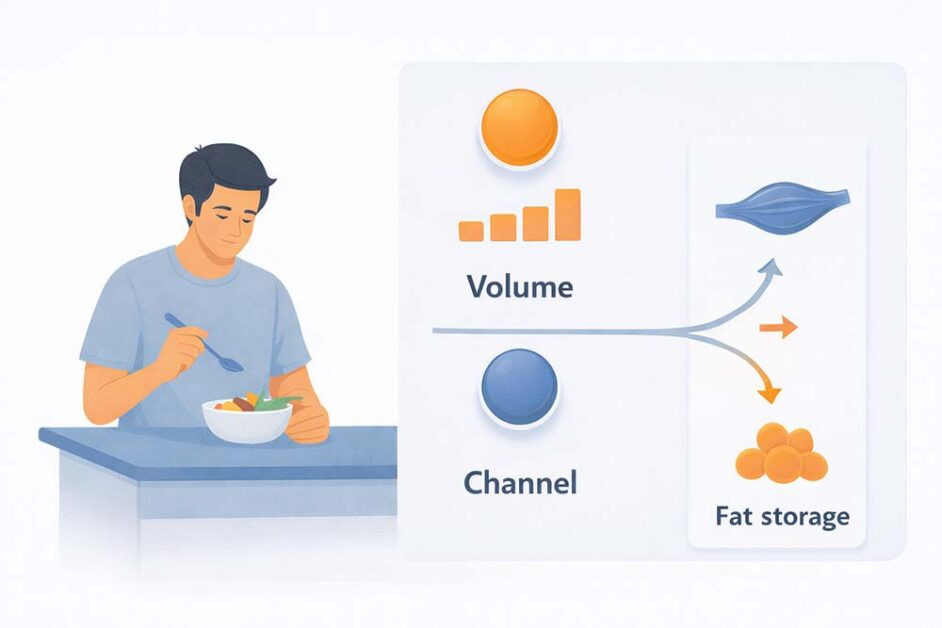
- Volume: How much insulin a meal demands. Large portions of refined carbohydrates push this button hard, forcing the body to release more insulin to manage blood sugar.
- Channel: Where glucose is directed after a meal. When muscle mass is low and meals lack protein or fibre, glucose is more likely to be stored as fat instead of being used for energy.
From years of observing how dietary advice is interpreted in real life, sustainable improvement comes from calming the system, not shocking it. That is how dietary change supports insulin resistance reversal without extremes.
Step 3️⃣ – Fixing the Protein & Fibre Gap
Dietary patterns in India create a unique metabolic challenge. Insulin resistance often appears at lower body weight because meals are energy-dense but protein-poor. The issue is not excess food alone. It is imbalance over time.
Why Indians Develop Insulin Resistance at Lower Body Weight
Traditional Indian plates are often carb-heavy by default. In many diets, 60–70% of daily calories come from refined cereals such as white rice and wheat rotis. Protein intake frequently stays around 10–12%, while fibre intake remains inconsistent. This imbalance drives repeated glucose spikes.
At the same time, resistance training is rare in daily routines. Muscle mass stays low even in people who appear lean. With less muscle available to absorb glucose, insulin must work harder to keep blood sugar stable.
Chronic protein deficiency compounds the problem. Without enough protein, muscle is not built or maintained. Satiety drops. Cravings rise.
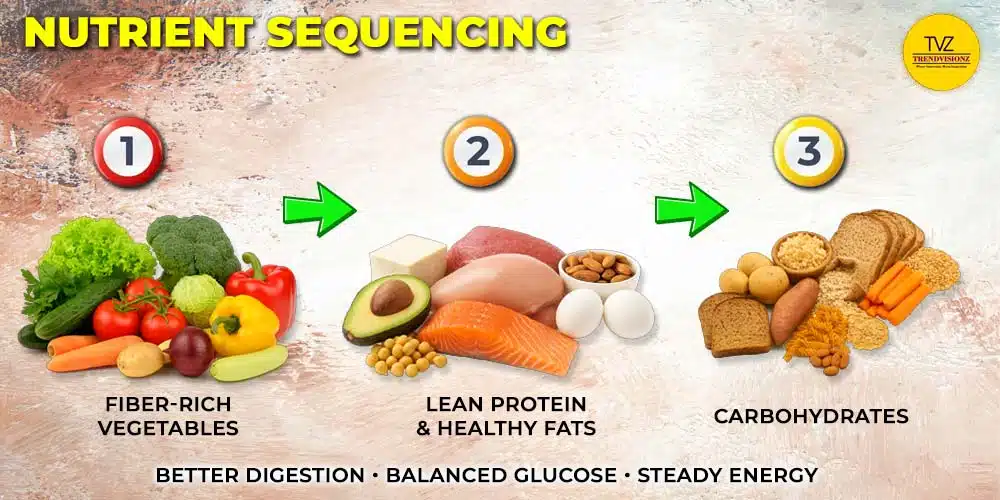
Food Sequencing That Works
How food is eaten matters as much as what is eaten. A simple nutrient sequencing pattern reduces insulin load without restriction.
“If you want to reverse insulin resistance naturally, three habits matter most. Food sequencing. Resistance training. And tracking your glucose response.” — Abhinav Mahajan, Fitness Expert
This approach works because it restores balance, not control. Starting meals with fibre, followed by protein and fats, and keeping carbohydrates for last slows digestion and flattens glucose spikes. Building muscle increases glucose uptake with less insulin. Consistency matters more than perfection.
Step 4️⃣ – Morning Routine & Circadian Reset
Insulin resistance is influenced not only by food and movement, but also by timing. The body runs on a circadian rhythm that governs hormones, digestion, and glucose handling. When this rhythm is disrupted, insulin efficiency drops, even if diet quality appears reasonable. Resetting the morning routine is one of the most underused tools for improving insulin sensitivity.
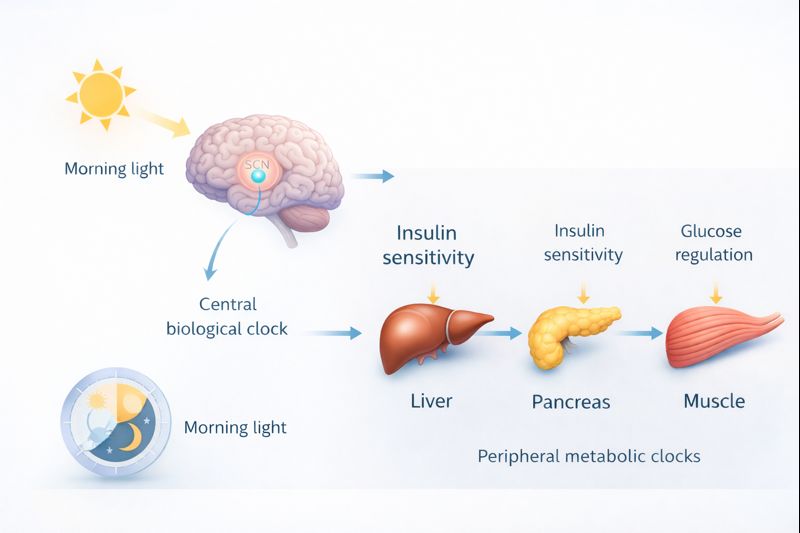
Light, Movement, and First-Meal Timing
Morning light is the primary signal that sets the body clock. Exposure to natural light soon after waking helps anchor the cortisol peak, which supports alertness, energy regulation, and healthy glucose metabolism.
Light movement in the morning reinforces this reset. A short walk, mobility work, or gentle activity primes muscles to absorb glucose later in the day. First-meal timing also matters.
“Time-restricted eating4 (TRE) works best when it follows the body’s circadian rhythm. Ending meals earlier in the evening and eating in morning naturally creates a 12–14 hour overnight fasting window”
Why does insulin work better earlier in the day?
Because insulin sensitivity follows the circadian rhythm. In the morning, cells respond more efficiently to insulin, allowing glucose to be cleared with less hormonal effort. Morning light reinforces this rhythm by setting a strong cortisol peak. Eating late, especially at night, pushes meals into a phase when insulin sensitivity is reduced.
Ending dinner earlier naturally creates a 12–14 hour overnight gap. Combine it with morning light, movement, and food timing. The reset improves insulin sensitivity and supports insulin resistance reversal without stress.
Step 5️⃣ – Sleep as Physical Metabolic Recovery
Sleep is often treated as passive rest. In reality, it is active metabolic repair. During deep sleep, the body recalibrates insulin sensitivity, clears stress hormones, and restores cellular energy balance. When sleep is disrupted, these repair cycles are shortened, and glucose regulation suffers.
Can poor sleep alone raise HbA1c?
Yes. Poor sleep can raise HbA1c on its own. The primary driver is cortisol. Sleep deprivation keeps cortisol elevated for longer periods, especially into the morning. Elevated cortisol directly interferes with insulin signalling, making cells less responsive to insulin.
“When you don’t sleep, your body’s ability to process sugar drops dramatically. An HbA1c of 6.0 is often a reflection of tired cells, not just bad diet.”- Matthew Walker, Sleep Scientist
From years of observing how metabolic data is interpreted in healthcare settings, I have seen sleep dismissed as optional. Yet stable sleep lowers cortisol and improves insulin sensitivity. When HbA1c rises, recovery should be examined first. Better nights often move markers faster than dietary changes.
Step 6️⃣ – Gut Health, Inflammation & Insulin Signalling
Insulin resistance is not driven by glucose alone. Chronic, low-grade inflammation 5plays a central role in how effectively insulin works at the cellular level. Much of this inflammation originates in the gut and is shaped by what is eaten consistently.
Why Inflammation Blocks Insulin Action
The gut is a major regulator of metabolic signalling. When fibre intake is low, beneficial gut bacteria decline. This weakens the intestinal barrier and allows inflammatory compounds to enter circulation.

How does gut-driven inflammation affect metabolism?
Inflammation interferes directly with insulin signalling. Cells become less responsive to insulin’s message, not because insulin is absent, but because inflammatory pathways block the signal. Glucose remains in the bloodstream longer, forcing the pancreas to release more insulin to compensate.
A fibre-deficient diet worsens insulin resistance by fuelling gut inflammation and erratic glucose absorption. From healthcare research, I have seen that fibre and gut health are overlooked.
Inflammation and Metabolic Slowdown
Gut-driven inflammation also affects how efficiently the body produces and uses energy. Fat oxidation reduces. Muscle recovery slows. The body shifts into a conservation mode where insulin resistance acts as a protective response rather than a failure.
People focus on calories and sugar while overlooking fibre and gut health. Yet improving gut balance often leads to better glucose control without extreme dietary change. Supporting gut health through fibre-rich, diverse foods becomes a foundational step in insulin resistance reversal.
Step 7️⃣ – Stress, Cortisol & Hormonal Load (Daytime Regulation)
Stress is not just an emotional experience. It is a physiological signal that directly affects glucose and insulin behaviour. In modern workdays, stress exposure is frequent, prolonged, and rarely resolved, creating a hormonal environment that quietly sustains insulin resistance.
Why Chronic Stress Keeps Insulin High
Chronic stress keeps the body in a constant alert state, repeatedly raising glucose and insulin levels even when no physical threat is present.
- Cortisol–glucose loop: Chronic stress raises cortisol, which increases blood glucose. Insulin rises repeatedly to compensate.
- Workday amplification: Prolonged sitting, mental pressure, constant notifications, and irregular meals keep this loop active all day.
- Hidden insulin load: Blood sugar may appear normal, but insulin remains persistently high, driving fatigue, cravings, abdominal fat, and worsening insulin resistance.
Nervous System Reset Practices
Simple nervous system resets lower daily stress load. Short breathing exercises, regular micro-breaks, brief walks, and consistent routines calm cortisol signalling. When stress reduces, insulin demand falls, glucose stabilises, and metabolic regulation becomes easier to sustain.
Managing stress is not optional for metabolic health. When cortisol is regulated daily, insulin demand falls. This creates a calmer internal environment where insulin resistance reversal becomes sustainable, without force or extremes.
Step 8️⃣ – Supplements as Support (Not Substitutes)
Supplements can support insulin function, but they cannot replace foundational habits. Their role is to correct gaps created by modern diets, stress, and soil depletion. When used thoughtfully, they reduce friction in metabolic pathways.
Minerals That Support Insulin Function
In clinical nutrition discussions, menopause and wellcoach, like Nidhi Kakar often emphasise that mineral deficiencies quietly impair insulin signalling long before blood sugar shifts appear. Several minerals play supporting roles in glucose regulation.
- Magnesium: Supports insulin receptor activity and glucose transport into cells. Deficiency is common in insulin resistance and stress states.
- Chromium: Improves cellular response to insulin and helps stabilise post-meal glucose swings.
- Zinc: Essential for insulin storage and release from the pancreas. Also supports immune balance and inflammation control.
- Selenium: Supports antioxidant defence and thyroid-related metabolic efficiency. Dose-sensitive and should not be overused.
- Phosphorus: Involved in cellular energy production and glucose metabolism. Low levels can reduce metabolic efficiency.
Supplements work best when correcting a true gap. They support insulin function, but only after movement, diet, sleep, and stress are addressed.
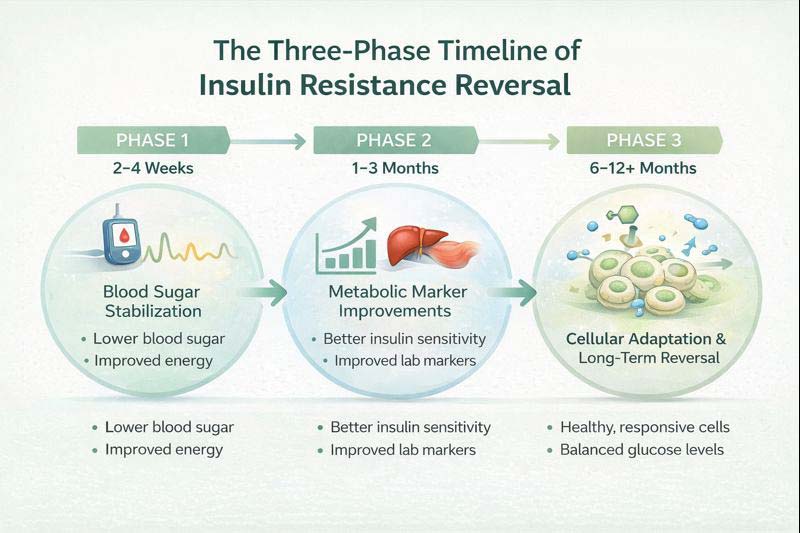
What to Expect While Reversing Insulin Resistance
Reversing insulin resistance is not a single action or a fixed timeline. It involves understanding which tools help, how long the body takes to respond, and how to recognise progress before visible weight loss occurs.
How Fasting Fits — and Where It Doesn’t
Intermittent fasting can reduce insulin resistance by lowering insulin exposure. It works best when built on stable sleep, movement, and nutrition rather than used as a standalone or extreme strategy.
“Insulin levels only come down when you stop eating long enough for them to fall. Constant snacking keeps insulin high all day.” — Dr Pradip Jamnadas, Founder and Medical Director of Cardiovascular Interventions
This explains why fasting can help. When food intake pauses long enough, insulin has space to fall. That break allows cells to regain sensitivity.
Used appropriately, fasting supports insulin sensitivity. Used too early, it adds stress. For most people, a natural 12–14 hour overnight gap delivers benefits without fatigue or metabolic strain.
How Long Does Insulin Resistance Reversal Really Take?
Insulin resistance reversal usually takes about 12 weeks, or roughly three months. This timeline aligns with HbA1c biology, which reflects average glucose exposure over the previous 8–12 weeks, not short-term dietary or weight changes.
“You don’t reverse insulin resistance by chasing the scale. You reverse it by restoring how cells respond to insulin over time.” — Stacey Burgess
True reversal follows cellular repair, not rapid weight loss. When expectations match biology, consistency replaces frustration. Over weeks, insulin signalling improves quietly, energy stabilises, and lab markers begin to reflect the deeper metabolic repair already underway.
Recognising Progress Before the Scale Moves
Weight is a delayed marker of metabolic health. Insulin resistance often begins improving long before the scale responds. Learning to recognise early signals prevents premature course correction.
5 Signs You’re Reversing Insulin Resistance
- Longer gaps between meals: Hunger becomes calmer and more predictable.
- Fewer cravings: Especially for refined carbohydrates and late-night snacks.
- Waist reduction: The waistline begins to shrink even if body weight stays stable. A healthy target is below 35 inches for women and below 40 inches for men, reflecting loss of visceral fat rather than muscle.
- Improved skin quality: Fewer breakouts and less inflammation as metabolic stress reduces.
- Sharper focus and steadier energy: Better mental clarity and fewer afternoon crashes.
These signs indicate that insulin demand is falling and cells are responding more efficiently. Progress in insulin resistance reversal is often felt before it is seen. When these markers improve, the system is healing, even if the scale has not caught up yet.
Also Read:
- The Complete Guide to Abortion Care: Safety, Science, and Global Context
- Kegel Exercises for Men & Women: Pelvic Health Guide
FAQs: Insulin Resitance Reversal
Can insulin resistance be reversed without medication?
Yes. In many cases, insulin resistance improves through lifestyle-first changes such as regular movement, adequate protein and fibre intake, improved sleep, and stress regulation. Medication may support some individuals, but reversal often begins with behaviour, not drugs.
Why do triglycerides rise before blood sugar?
Triglycerides often rise first because excess glucose is converted into fat and stored in the liver. Insulin continues to keep blood sugar appearing normal, masking metabolic dysfunction long before fasting glucose or HbA1c levels increase.
Can insulin resistance exist with normal HbA1c?
Yes. Insulin resistance often develops years before HbA1c rises. During this stage, insulin levels remain high enough to control blood sugar, while metabolic stress builds silently through elevated insulin, triglycerides, and liver fat.
Conclusion
Insulin resistance sits at the root of many modern metabolic conditions, long before diagnoses like prediabetes or type 2 diabetes are made. The encouraging truth is that insulin resistance reversal is possible. It responds to consistent changes in movement, nutrition, sleep, and stress regulation.
A lifestyle-first approach works because it lowers insulin demand at its source instead of chasing symptoms. Small, repeatable habits matter more than intensity or extreme protocols. Over time, these signals restore insulin sensitivity, stable blood sugar, and overall metabolic health. Progress may feel slow, but it is cumulative and real.
When the focus stays on alignment rather than urgency, reversing insulin resistance becomes sustainable, not stressful.
If you’re looking to communicate health insights with clarity and scientific responsibility, TrendVisionz helps brands translate complex medical science into trusted, human-centred narratives that inform, not alarm.
Additional Resources:
- Zdrojewicz Z, Popowicz E, Szyca M, Michalik T, Śmieszniak B. TOFI phenotype – its effect on the occurrence of diabetes. Pediatr Endocrinol Diabetes Metab. 2017;23(2):96-100. doi: 10.18544/PEDM-23.02.0079. PMID: 29073292. ↩︎
- Adeva-Andany MM, Pérez-Felpete N, Fernández-Fernández C, Donapetry-García C, Pazos-García C. Liver glucose metabolism in humans. Biosci Rep. 2016 Nov 29;36(6):e00416. doi: 10.1042/BSR20160385. PMID: 27707936; PMCID: PMC5293555. ↩︎
- Merz KE, Thurmond DC. Role of Skeletal Muscle in Insulin Resistance and Glucose Uptake. Compr Physiol. 2020 Jul 8;10(3):785-809. doi: 10.1002/cphy.c190029. PMID: 32940941; PMCID: PMC8074531. ↩︎
- Mishra S, Persons PA, Lorenzo AM, Chaliki SS, Bersoux S. Time-Restricted Eating and Its Metabolic Benefits. J Clin Med. 2023 Nov 9;12(22):7007. doi: 10.3390/jcm12227007. PMID: 38002621; PMCID: PMC10672223. ↩︎
- Tsalamandris S, Antonopoulos AS, Oikonomou E, Papamikroulis GA, Vogiatzi G, Papaioannou S, Deftereos S, Tousoulis D. The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives. Eur Cardiol. 2019 Apr;14(1):50-59. doi: 10.15420/ecr.2018.33.1. PMID: 31131037; PMCID: PMC6523054. ↩︎
Stay Connected with Me:
Anuj Mahajan is a marketing and communication professional with over 30 years of experience. A senior business and media operator, he uses storytelling to bring clarity, strengthen communication, and reinforce leadership discipline to drive growth. He is an ICF-ACC Certified Coach and an experienced corporate trainer. Drawing from deep operating experience, he helps leaders and organizations translate strategy into consistent business outcomes.
- Explore my work: Nuteq Entertainment | TrendVisionz | Author Profile
- Read our newsletters: Transforming Lives | BizTech Chronicle | Nuteq Newsline
- Guest writer: BizCatalyst360 | Praja Today
- Books: Go Mindfulness: Practices for Professionals Coached
- Join the community: LinkedIn Group – Digital Marketing & Content Creation World
- Connect with me: LinkedIn | Twitter | #StoryforBusiness
- Share your review: Leave your review on Google — your feedback helps us grow.
- Listen on Spotify: Leadership Podcast | Guided NLP (7 Episodes) | Daily Motivation – 21 Episodes
Believe. Practice. Perform. Let’s create impact together.
✍️ A Note from the Editor
Independent storytelling thrives with you. Contribute $15/month via PayPal or email us at anujmahajan@trendvisionz.com. [Guest write for us — Free or Paid.]





3 comments
Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others
Nice post. I learn something totally new and challenging on websites
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
Comments are closed.