We panic if our laptop fan makes a little too much noise, yet we ignore the fact that our body’s internal CPU, the liver, is overheating every day. You can replace a burnt-out processor. You cannot simply reboot your metabolism. Across Corporate India, liver health is quietly declining as sedentary lifestyle, long working hours, work stress, and poor sleep become normalised in modern office environments.

A recent study has revealed that around 84 percent1 of Indian IT professionals show signs of fatty liver disease. What makes this alarming is that fatty liver is no longer linked only to alcohol. Imagine a highway where cars keep entering, but no one is allowed to exit. That is your liver on a sedentary workday, with energy coming in but nowhere to go.
From my 32 plus years in media and corporate training, I have seen how back-to-back meetings, long screen hours, and constant availability reshape daily habits without notice. Over time, these patterns strain metabolic health and increase the risk of fatty liver in office workers.
This article explores how long work hours and sedentary habits damage liver health, the early warning signs professionals often overlook, and practical steps that fit real corporate lives.
Also Read:
- The Modern Fauji Wife: Entrepreneurs of Grace and Grit
- Everyday Skincare for Urban Living and Busy Lifestyles
The Silent Epidemic of Fatty Liver in Professionals
Fatty liver is still widely perceived as an alcohol-related condition. In reality, it has become one of the most common lifestyle-driven health risks among professionals. The shift is subtle but serious. Liver health is declining.
“Fatty liver disease is not just fat in the liver. It is a metabolic warning sign. Excess fat disrupts liver function and, if ignored, can progress to inflammation, fibrosis, cirrhosis, and even liver cancer. It is also strongly linked to type 2 diabetes, heart disease, and PCOS.” — Dr. Piyush Gupta, Gastroenterology, Max Hospital

Incidence of Fatty Liver in Office Workers
Modern office environments unintentionally promote liver dysfunction. Long hours at a desk, when energy intake consistently exceeds energy use. The liver becomes the primary storage site, leading to fat accumulation and metabolic stress even in non-drinkers.
- Fatty liver without alcohol: Today, fatty liver is largely driven by insulin resistance and metabolic overload.
- Desk jobs and lifestyle: Sitting for eight or more hours slows lipid oxidation, redirecting excess calories into liver fat storage.
- Early impact on liver health: Clinicians are now detecting inflammation and early fibrosis in professionals in their early thirties.
Why This Epidemic Goes Unnoticed
Fatty liver progresses quietly like a silent epidemic. The liver has no pain receptors, so damage builds without obvious symptoms. Many professionals assume they are healthy because they have a normal BMI. In reality they allow internal metabolic dysfunction to go unchecked.
- Silent progression: There is no early pain or discomfort to raise alarms.
- Normal-weight individuals at risk: Being “skinny fat” allows visceral liver fat to accumulate despite outward fitness.
- Missed screening: Standard corporate health check-ups often skip liver imaging and fibrosis markers.
What makes lifestyle-related health decline dangerous is how normal it feels while it is happening. Many professionals only recognise the impact years later, when energy, focus, and resilience begin to fade.
“Sitting through long hours without breaks felt normal in sales leadership. Over time, constant screen focus, irregular meals, and skipped movement quietly drained my energy, focus, and overall health more than I realised.” — Rekha Sharma, Sales and Marketing Strategist, Manroland
The silent progression becomes clearer when viewed at scale. The numbers reveal how widespread and underestimated this workplace-driven health crisis has become.
Why Are the Numbers So Alarming?
While academic studies establish prevalence, a recent cover report by Palki Sharma on Firstpost places the crisis in a broader national and global context. The concern is not just prevalence, but who is being affected and why.
- India records over 268,000 liver disease deaths annually. Accounting for more than 3 percent of all deaths and over 18 percent of global liver-related fatalities.
- Non-alcoholic fatty liver disease affects nearly 38 percent of Indian adults. The prevalence rising even among children and young professionals.
- One in three Indians is now estimated to have NAFLD. Driven by physical inactivity metabolism
- Lifestyle-related liver disease is increasingly seen in the 35–54 age group. Aligning closely with long working hours, desk jobs, and chronic work stress.
Takeway: These data signals a sobering reality. For today’s professionals, the office chair and long workday are emerging as serious threats to liver health. Fatty liver behaves like a corrupted background app. Long workdays and inactivity fuel the damage quietly, until the body forces a shutdown you cannot ignore.
How Long Work Hours Damage Your Liver
Extended working hours in offices often do more than reduce personal time. Prolonged sitting2 at workplace quietly alter liver function. Recovery time shrinks, stress responses rise, and metabolic balance weakens. When workdays stretch without meaningful breaks, the liver remains in a state of continuous load rather than repair.
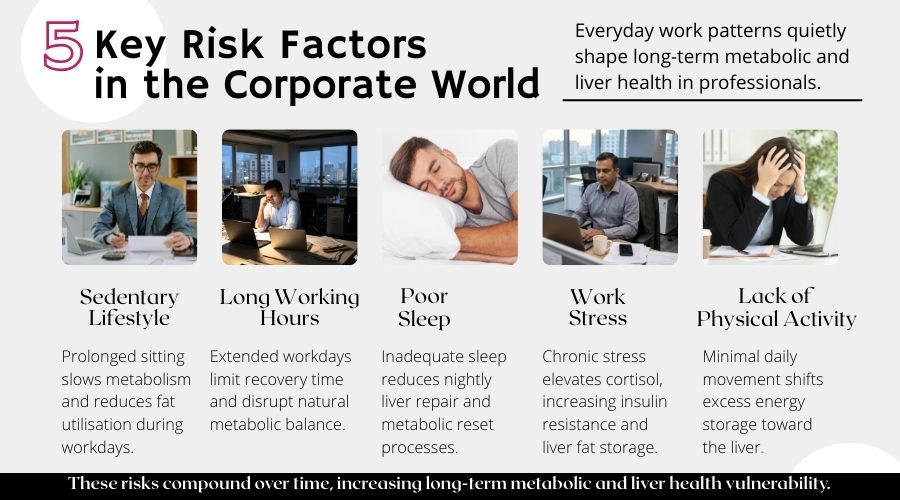
Work Stress and Metabolic Health
Chronic work stress keeps the body in a prolonged alert state. Elevated cortisol interferes with insulin sensitivity, pushing the liver to convert excess circulating glucose into stored fat. Over time, this stress-driven metabolic shift increases liver fat accumulation even in people who eat moderately and avoid alcohol.
From my own experience, I personally sit for long hours and genuinely enjoy it. I multitask constantly and thrive in high-intensity work environments. What helped me sustain this was the Pomodoro method. Structured breaks improved my focus and kept me from sitting continuously, while maintaining the same
Sleep Deprivation and Liver Recovery
Sleep is when the liver performs most of its detox and repair work. Late-night work, irregular schedules, and constant screen exposure delay this process. When sleep is shortened or fragmented, metabolic repair remains incomplete, increasing inflammation and reducing the liver’s ability to recover from daily strain.
Many professionals assume five or six hours of sleep is enough. Over months and years, this deficit compounds, weakening liver resilience and slowing metabolic recovery.
Do long working hours affect liver health?
Yes. Extended work hours combine stress overload, reduced sleep, and limited recovery time. Together, these factors disrupt hormonal balance, slow metabolism. The liver shifts toward fat storage instead of repair, raising long-term health risks.

“What helped me most was redefining consistency. I stopped chasing perfect routines and focused on small non-negotiables like daily walks and fixed shutdown times. These habits restored energy and clarity without affecting delivery or leadership outcomes.” — Krishna Ghosh, Global Delivery Leader, IBM
Takeway: Remember this, long work hours are not the enemy. Ignoring recovery is. With conscious breaks, better sleep, and awareness, professionals can protect liver health without sacrificing focus, ambition, or productivity.
Waistline as a Warning Sign
An expanding waistline 3is often the earliest visible indicator of declining liver health. Unlike overall body weight, waist circumference reflects the build-up of visceral fat around internal organs, including the liver. This hidden fat is metabolically active and closely linked to insulin resistance and fatty liver disease.
Why Waist Circumference Matters More Than BMI
Medical evidence shows that waist circumference is a more practical and reliable screening marker for fatty liver risk than Body Mass Index. Many professionals maintain a normal BMI while accumulating visceral fat. This explains why fatty liver is increasingly diagnosed in people who appear lean but have lack of physical activity. The condition is now referred to as Metabolic Dysfunction–Associated Steatotic Liver Disease (MASLD).
Recommended Waistline Limits
Health professionals rely on waist circumference as a simple, early screening tool to flag metabolic and liver risk. Unlike weight or BMI, it reflects harmful visceral fat accumulation and helps identify fatty liver risk before symptoms or lab abnormalities appear.
For men:
A waist circumference above 94 cm or 37 inches signals increased risk. Some guidelines suggest lower cutoffs for earlier detection in high-risk groups.

For women:
A waist circumference above 80 cm or 31.5 inches increases metabolic and liver risk, with lower thresholds advised in some cases.
What Early Signs Should Professionals Watch for?
Fatty liver often progresses silently. When symptoms appear, they may include persistent fatigue, mild upper-right abdominal discomfort, digestive issues, or darkened skin patches linked to insulin resistance. These signs usually surface late.
Waistline acts as an early dashboard warning for corporate professionals. Tracking it offers a simple, visible cue to address liver health before silent damage turns into disease.
The Dangerous Progression of Fatty Liver Disease
Fatty liver disease is often dismissed as a minor or reversible finding. In reality, it can progress into serious liver damage 4when lifestyle risks continue unchecked. What begins as fat accumulation can quietly evolve into inflammation, scarring, and irreversible liver disease.
Early Stage Fatty Liver Disease
In the early stage of fatty liver disease, fat accumulates inside liver cells without causing noticeable symptoms. Blood reports may still appear normal, which often delays attention. This stage is critical because liver damage is still reversible with timely lifestyle intervention.
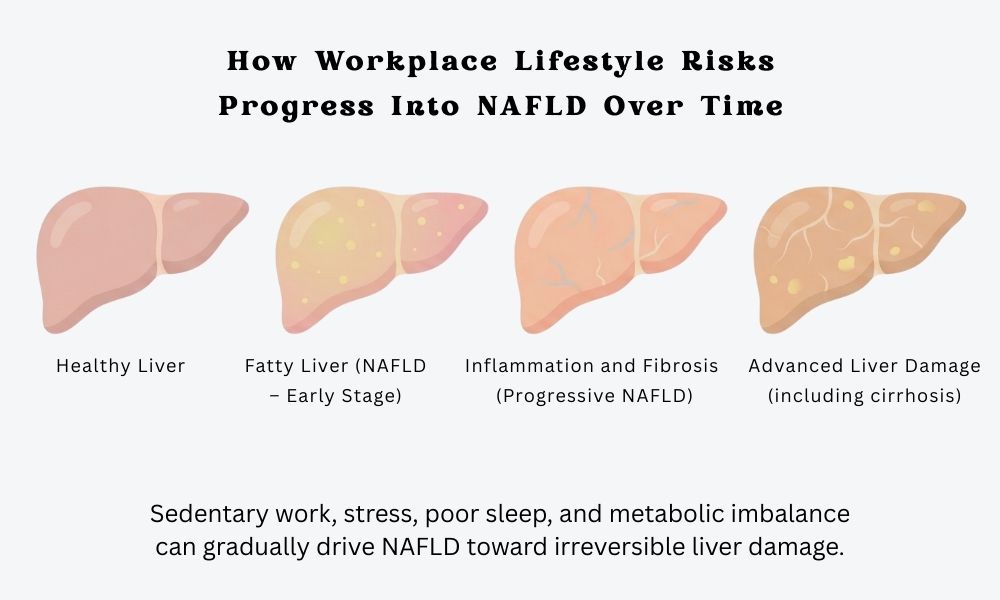
• Silent fat accumulation: Excess fat builds up in liver cells without pain or discomfort.
• Normal test results: Routine liver function tests may not detect early damage.
• Lack of symptoms: Most individuals feel healthy despite underlying metabolic stress.
• Early metabolic disruption: Insulin resistance and fat metabolism begin to worsen.
• Window for reversal: Lifestyle correction can still clear stored fat and restore liver health.
The greatest risk at this stage is false reassurance. Without awareness and early action, fatty liver can progress quietly into more serious disease.
When Lifestyle Diseases Advance
If metabolic stress persists, fatty liver begins to progress. Lack of movement slows metabolism. Over time, this leads to fibrosis, where healthy liver tissue is replaced with scar tissue.
According to the World Health Organization, hepatitis remains a major global liver health concern, contributing to long-term liver damage and preventable mortality.
Hepatitis is a major public health problem and can cause liver inflammation, fibrosis, cirrhosis, and liver cancer — World Health Organization (WHO)
As lifestyle diseases such as diabetes and obesity advance, liver damage accelerates. As damage continues, the liver struggles to heal itself, increasing the chances of long-term scarring and serious liver disease. At this stage, reversal becomes far more difficult.
What is Stage 1 liver disease?
Stage 1 liver disease refers to early fatty liver without significant scarring. It is largely reversible with early intervention, making timely lifestyle changes and medical monitoring critical to prevent long-term damage.
Practical Steps to Protect Your Liver
Protecting liver health does not require extreme fitness routines or rigid diets. For most office professionals, consistent small changes matter more than dramatic interventions. When daily habits support movement, stress regulation, and recovery, the liver gets the space it needs to repair and function efficiently.
Movement and Physical Activity at Work
Regular movement during the workday is one of the most effective ways to counter prolonged sitting. Even brief activity breaks help restart metabolic processes that stall during desk-bound hours.
- Break long sitting cycles: Stand or move for a few minutes every hour to restart circulation.
- Add movement to routine tasks: Walk during calls or meetings where possible.
- Use micro-movements: Stretching, stairs, or short walks reduce metabolic stagnation without disrupting work.

Managing Work Stress and Sleep
Stress control and sleep consistency are critical for liver recovery. Chronic stress keeps metabolic systems overactive, while poor sleep reduces the liver’s ability to repair daily damage.
- Manage stress proactively: Short breathing breaks, structured pauses, or mindfulness practices reduce cortisol load.
- Protect sleep timing: Aim for consistent sleep hours, even during busy work phases.
- Support metabolic balance: Adequate rest improves insulin sensitivity and reduces inflammation.
This shift toward balance is already visible across corporate India. Many professionals are recognising that long-term performance depends on sustainable routines, not constant pressure. Small, consistent changes in stress and sleep habits often become the turning point.
“Health is not built in dramatic bursts, but in daily discipline. Small actions, repeated consistently, shape strength, resilience, and longevity far more than occasional effort.” — Tilak Amitava Chowdhury, Marketing and Communications Lead, AECOM
When movement, stress, and sleep are managed together, liver protection becomes practical and sustainable. These habits fit real corporate lives and deliver long-term health benefits without compromising performance or ambition.
Also Read:
- Budget Fashion Hacks to Look Expensive Every Day
- Boost Fitness with Japan’s 3-Minute Interval Walking Routine
- Kegel Exercises for Men & Women: Pelvic Health Guide
FAQs : Liver Health
How many hours of sitting are unhealthy per day?
Sitting for more than 7–8 hours a day without regular movement increases metabolic stress and fatty liver risk. The issue is not total sitting alone, but long uninterrupted sitting without breaks or muscle activity.
Can small daily habits really reverse fatty liver?
Yes. Early-stage fatty liver is often reversible through consistent habits such as regular movement breaks, improved sleep, stress control, and metabolic awareness. Dramatic routines matter less than small actions repeated daily.
What is the Pomodoro technique and how does it support liver health?
The Pomodoro technique breaks work into focused intervals with short movement breaks. These pauses reduce prolonged sitting, lower stress load, and support metabolic activity, making it a practical tool for protecting liver health at work.
Why do professionals develop fatty liver despite eating normally?
Fatty liver in professionals often develops due to long working hours combined with minimal physical activity. When muscles are not regularly engaged, even moderate calorie intake can exceed daily energy use, promoting fat storage in the liver over time.
Conclusion
Modern work culture has quietly reshaped how professionals live, move, and recover. Long working hours, sedentary lifestyle patterns, stress and metabolic health now form a daily routine that steadily undermines liver health in office workers.
Fatty liver disease has become common across corporate environments, but it is not inevitable. When identified early, fatty liver is often reversible through awareness, regular screening, and small daily lifestyle adjustments that support metabolic health. The key lies in noticing early warning signs and acting before silent damage progresses.
Protecting liver health does not require extreme routines, only consistency and intent. If organisations want sustainable performance, employee health must be part of the conversation.
At TrendVisionz, we continue to highlight workplace health realities to encourage informed choices. We believe healthier work cultures and meaningful conversations are what ultimately lead to real change.
Additional Resources:
- Bhargava, B., Rao, P.N., Kulkarni, A.V. et al. Prevalence of metabolic dysfunction-associated fatty liver disease among information technology employees in India. Sci Rep 15, 10124 (2025). https://doi.org/10.1038/s41598-025-91482-2 ↩︎
- Hamilton, M. T., Healy, G. N., Dunstan, D. W., Zderic, T. W., & Owen, N. (2008). Too little exercise and too much sitting: Inactivity physiology and the need for new recommendations on sedentary behavior. Diabetes, 57(2), 265–271 ↩︎
- Zhang M, Zhao E, Sun G. Association between waist circumference and fatty liver disease in older adult population: a cross-sectional study in Urumqi. Front Public Health. 2025 Jul 8;13:1620261. doi: 10.3389/fpubh.2025.1620261. PMID: 40697841; PMCID: PMC12279773. ↩︎
- Younossi, Z. M., Golabi, P., de Avila, L., Paik, J. M., Srishord, M., Fukui, N., Qiu, Y., Burns, L., Afendy, A., & Nader, F. (2019). The global epidemiology of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology, 69(6), 2672–2682. ↩︎
Stay Connected with Me:
Anuj Mahajan is a Mass Communication Specialist, ICF-ACC Certified Coach, Corporate Trainer, Motivational Speaker, NLP Life Coach, Filmmaker, and Author. With 30+ years in media, marketing, and leadership coaching, he unites storytelling, mindfulness, and digital transformation.
- Explore my work: Nuteq Entertainment | TrendVisionz | Author Profile
- Read our newsletters: Transforming Lives | BizTech Chronicle | Nuteq Newsline
- Guest writer: BizCatalyst360 | Praja Today
- Books: Go Mindfulness: Practices for Professionals Coached
- Join the community: LinkedIn Group – Digital Marketing & Content Creation World
- Connect with me: LinkedIn | Twitter | #StoryforBusiness
- Share your review: Leave your review on Google — your feedback helps us grow.
- Listen on Spotify: Leadership Podcast | Guided NLP (7 Episodes) | Daily Motivation – 21 Episodes
Believe. Practice. Perform. Let’s create impact together.
✍️ A Note from the Editor
Independent storytelling thrives with you. Contribute $15/month via PayPal or email us at anujmahajan@trendvisionz.com. [Guest write for us — Free or Paid.]



7 comments
Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
Awesome! Its genuinely remarkable post. I have got much clear idea regarding from this post
Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
Impressive work—each point is articulated with strong professionalism.
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
thanks…stay connected
I appreciate you sharing this blog post. Thanks Again.
Comments are closed.